- related: OBGYN
Cervical cancer
The most appropriate screening strategy is to obtain the results of the patient's last cervical cancer screening examination. Both the U.S. Preventive Services Task Force (USPSTF) and the American Cancer Society (ACS) recommend against cervical cancer screening in women older than age 65 years who have had adequate prior screening and are not otherwise at high risk for cervical cancer. The USPSTF defines adequate screening as three consecutive negative cytology (Pap smear) results or two consecutive negative cytology plus human papillomavirus (HPV) test results within the last 10 years, with the most recent test occurring within 5 years. The ACS defines adequate prior screening within the prior 10 years as three negative cytology tests with the most recent test within 3 years, or HPV-based testing with the most recent test within the past 5 years (two negative combined cytology and HPV tests, or two negative primary HPV tests). Data suggest that cervical cancer screening rates decline with increasing patient age; however, a Kaiser Permanente registry study found that 13% of 65-year-old women have not been adequately screened, with higher rates in patients without a primary physician or other health care provider. Other populations that are less likely to have received adequate screening include women with limited access to care, women from racial or ethnic minority groups, and women from countries where screening is not available. The study also documented that most cases of invasive cervical cancer in women older than age 65 years occurred among those who had not met criteria for stopping screening. The decision to stop screening at age 65 years should only be made after confirming that the patient has received adequate prior screening. In patients who do not meet the criteria for adequate prior screening, screening may be clinically indicated after age 65 years.
Cervical cytology, high-risk HPV testing, or co-testing with cervical cytology and high-risk HPV testing may all be reasonable methods to screen for cervical cancer in this patient, but reviewing the adequacy of previous screening remains the first step in management.
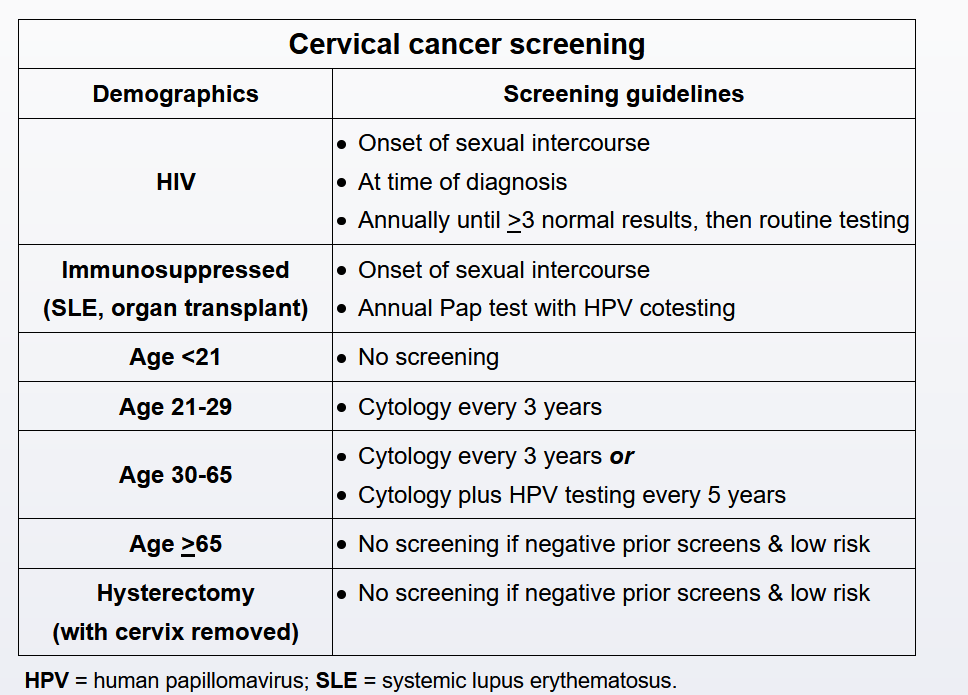
Cervical cancer is caused by persistent infection with high-risk strains (eg, type 16, 18) of human papillomavirus (HPV). Risk factors include early onset of sexual activity, multiple sex partners, tobacco use, and immunosuppression. Screening identifies patients with abnormal cytology/premalignancy and prevents progression to malignancy. Current screening guidelines include initiation of cervical cancer screening at age 21 irrespective of sexual activity (Choice A). In women age 21-29, screening is with Pap testing every 3 years. In women age 30-65, screening options include:
- Pap testing every 3 years OR
- Pap and HPV cotesting every 5 years OR
- Primary HPV testing every 5 years
Therefore, a patient age 30-65 who had a normal Pap test 3 years ago would need testing. In contrast, a patient who had a normal Pap and a negative HPV test 4 years ago would not (Choice B). Exceptions to these guidelines include patients who are HIV positive or immunosuppressed. These patients require screening at the time of diagnosis (HIV) or at the onset of sexual activity (immunosuppression) and require screening at more frequent intervals.